Learning as a System
Transforming clinical education into interactive experiences designed for patients, not just professionals.
The decision at risk
In the healthcare ecosystem, educational resources were historically designed for physicians.
Patients diverse in age, context and condition were secondary recipients of translated information.
If patient education continued to rely on traditional lecture formats, engagement and retention would remain low, especially across diverse age groups and clinical realities.
Why it was risky
Why this mattered
For patients with chronic conditions, education directly influences adherence, prevention and quality of life.
When information is delivered passively, fear and stigma can persist, leading to avoidance, low engagement and higher risk.
My point of view
Health education for patients must be experiential, not instructional.
Understanding, retention and behavioral adoption increase when learning is participatory and emotionally engaging.
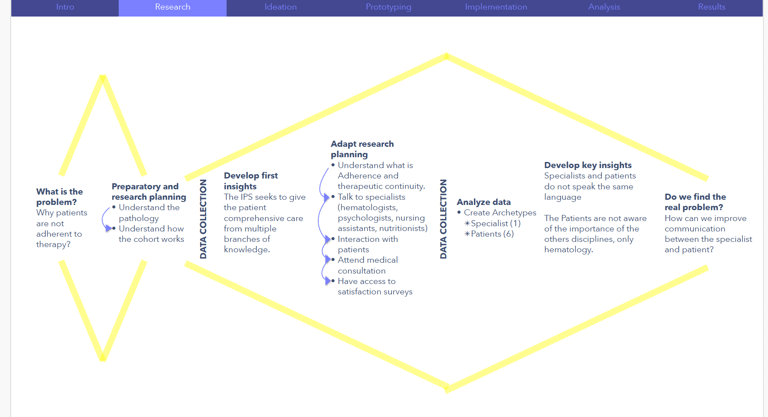
What I needed to understand
Deep-diving into each specific pathology to understand clinical implications, risks and daily-life impact.
Mapping the interdisciplinary care model (psychology, physiotherapy, nursing and medical specialties) to identify how each discipline contributed to patient support.
Conducting interviews and focus groups with patients and caregivers to uncover emotional, cognitive and behavioral barriers.
Translating clinical knowledge into accessible narratives and experiential dynamics.
Piloting adapted lecture formats to test comprehension and engagement.
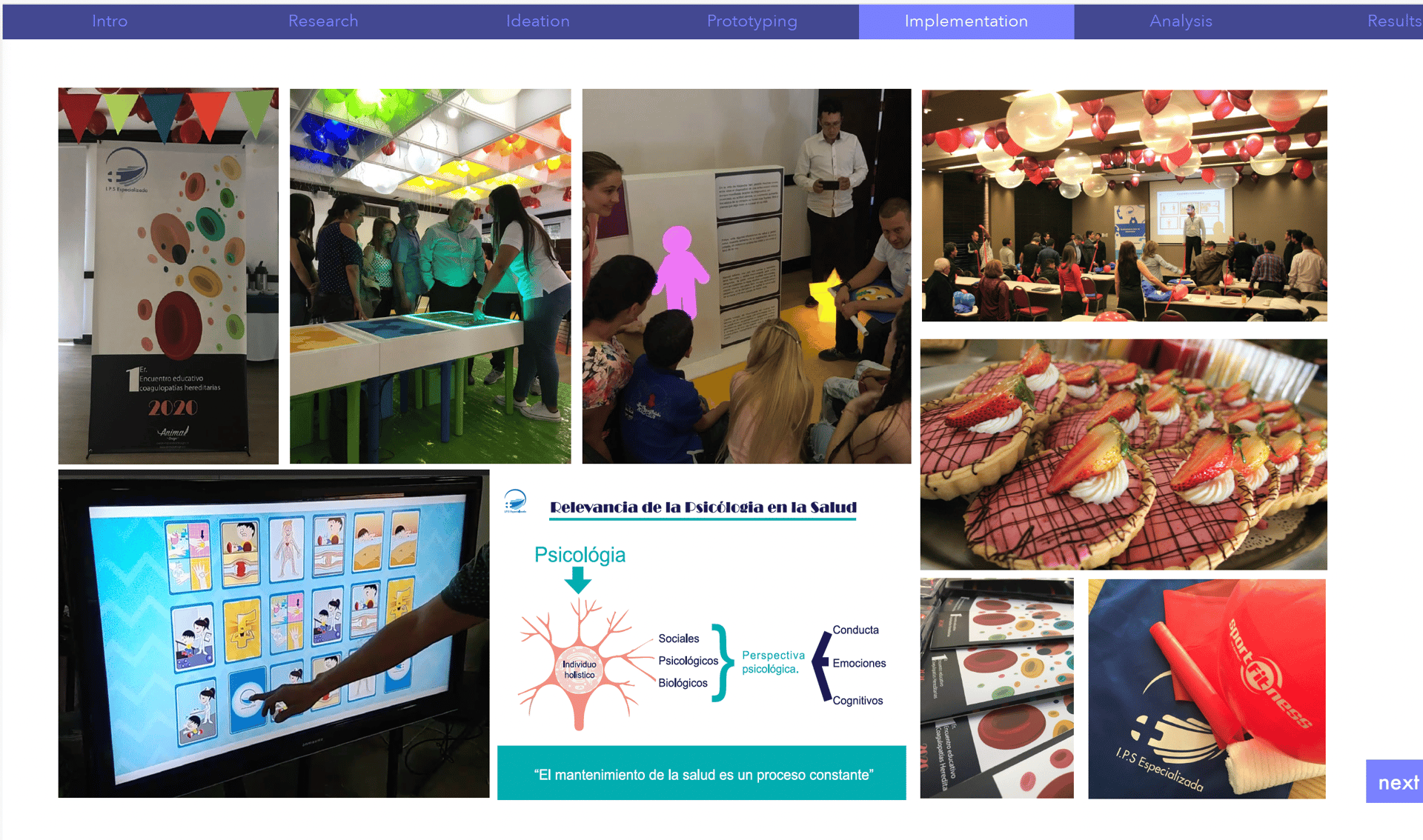
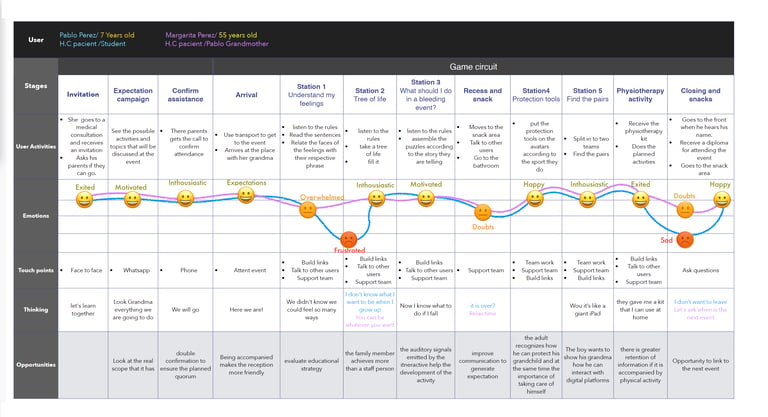
Designing hybrid events structured around 7 interactive stations, each representing a discipline within the integral care model.
Observing behavioral engagement and retention across diverse age groups.
How different age groups engaged with medical information
How caregivers influenced learning dynamics
What emotional and behavioral barriers existed around specific conditions
Whether traditional adapted lectures were enough to drive retention
How this was explored
What changed
Patient-centered experiential model
Hybrid interactive stations
Learning through participation and play
Higher engagement and knowledge retention across age groups
Physician centered educational model
Traditional lecture format
Information translated but still passive
Low behavioral reinforcement
Before
After
System impact
Patients demonstrated increased adherence to treatment protocols.
The narrative shifted from “being punished by a condition” to understanding how to manage risk proactively.
Both patients and caregivers showed stronger engagement and retention through experiential learning.
The initiative reframed the disease from identity, defining to manageable through informed prevention and empowerment.
Designing for patients requires embracing diversity in age, emotional state and cognitive needs.
What works for specialists does not necessarily work for lived experience.
Important trade-off
Experiential formats required more coordination, resources and cross-disciplinary alignment.
However, the increased engagement and retention justified the complexity.